As scientific research and computational analysis deepen our understanding of cell biology, we are moving toward the promise of precision cancer medicine. Using next-generation DNA sequencing to thoroughly scan the cancer genome, and large, data-intensive research projects like Profile to better understand the disposition and behavior of cancer cells, the team at Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC) is improving targeted treatments for cancer patients.

“We’re working to tackle the disease with multiple approaches geared specifically to that cancer so we can stop it for good,” says Jeffery A. Golden, MD, chief pathologist at Brigham and Women’s Hospital
“Cancer is very smart,” says Jeffery A. Golden, MD, chief pathologist at Brigham and Women’s Hospital. “If we address a single mutation with only one approach, cancer may find a way around it. We’re working to tackle the disease with multiple approaches geared specifically to that cancer so we can stop it for good.”
The goal of precision cancer medicine, explains Bruce Johnson, MD, chief clinical research officer at Dana-Farber Cancer Institute, is to see the whole picture of an individual patient.
So, in addition to systematically genotyping tumor tissue from most patients at DF/BWCC to help guide therapies focused on malignant tumors, research and clinical teams have expanded the field of precision cancer medicine by discovering and testing a number of other approaches and techniques. Some of the most promising are described here.
Basket Trials: Another Twist on Clinical Trials
Currently, most clinical trials in this area are genotyping studies in which participants have the same type of cancer. Today, we are exploring “basket” trials that seek to match patients with similar mutations, rather than by the location of their cancer. A recent study of one patient’s dramatic response to a targeted therapy has led investigators to open such a trial to test the effectiveness of the drug in other patients with the same mutation.
In 2010, a 56-year-old woman was diagnosed with anaplastic thyroid cancer, a form of cancer that is almost always fatal within a few months. Despite surgery, radiation, and chemotherapy, the tumor spread to her lungs. In an attempt to stem the tide of the disease, she was enrolled in a clinical trial of everolimus, which has been showing promise as a targeted therapy for a number of cancers, including a treatable type of thyroid cancer.
In a surprise response, the patient’s tumor shrank and remained that way for 18 months before it began to grow again. Using whole-exome DNA sequencing, which scans the protein-coding regions of the genome, the investigators discovered a mutation in the TSC2 gene. This mutation caused the patent’s exceptional response to the target treatment. Because of this patient’s response, the clinical trial was expanded to include others who have been identified with the TSC2 gene mutation.
Cancer Immunotherapy and Vaccines
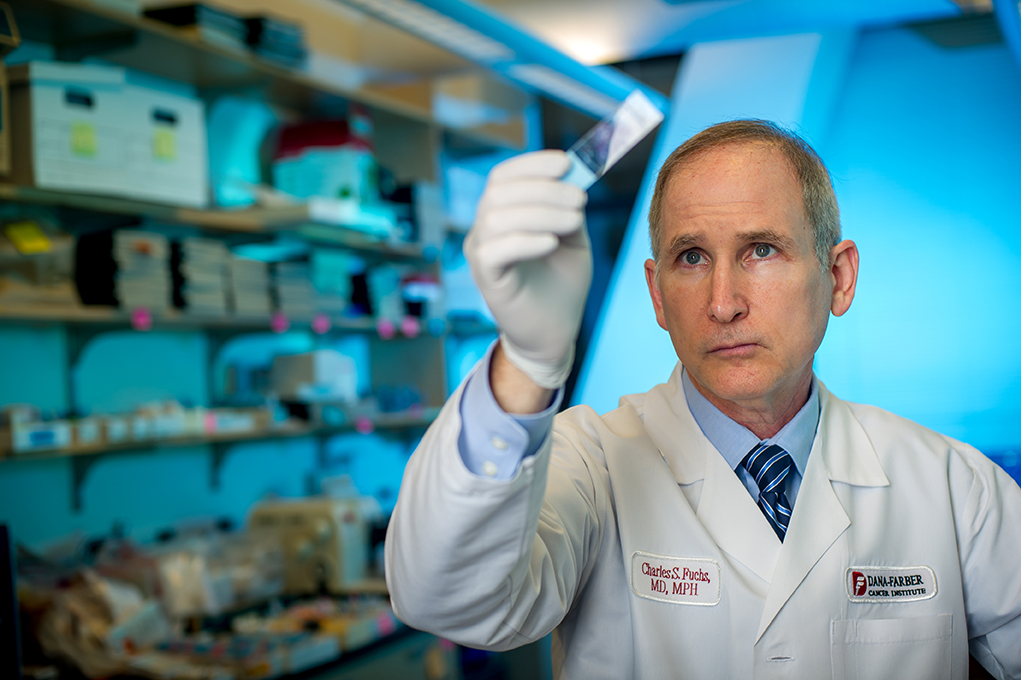
In the laboratory, Dr. Charles Fuchs, MD, MPH, director of the Center for Gastrointestinal Cancer, focuses on biochemical markers of gastrointestinal cancer risk, molecular predictors of patient prognosis in colorectal and pancreatic cancers, and the discovery of novel targets for cancer therapy.
Cancer immunotherapy, which mobilizes the body’s own immune system to fight disease, is a particularly promising area of research. Immunotherapy includes a variety of treatments that work in different ways: some are intended to boost the immune system defenses in a general way; others help train the immune system to recognize and attack cancer cells specifically. So far, it appears that this type of treatment works better for some types of cancer than others.
Currently, clinical research at the DF/BWCC Hematologic Oncology Center is studying agents known as “immune checkpoint inhibitors,” which interfere with the body’s natural immune defenses. PD-1 is a checkpoint pathway that plays a key role in modulating the immune system. However, some cancers exploit this pathway to evade the body’s immune defenses. In particular, a study of a PD-1 (programmed death 1) blockade in Hodgkin lymphoma has led to the FDA bestowing breakthrough status on this promising therapy.
The Center is also studying a new type of vaccine to boost the body’s immune response to melanoma. Melanomas have mutations that are specific to an individual patient, and which can cause the tumor cells to produce proteins that appear very different from the body’s own cells. The study is evaluating the making and administering of a safe vaccine by using information gained from specific characteristics of the participant’s own melanoma.
Identifying Risk Factors
Cancer cells in culture from human connective tissue, illuminated by darkfield amplified contrast, at a magnification of 500x (Courtesy of the National Cancer Institute)
Considerable work is also underway to predict biological identifiers that might indicate a predisposition to cancer in some people. At the DF/BWCC Pancreaticobiliary Tumor Center, researchers are conducting clinical trials to identify risk factors and biomarkers for pancreatic cancer. Because there are currently very few early warning signs of pancreatic adenocarcinoma, a diagnosis is often made only when the disease is advanced.
Researchers have found that elevated metabolites (branched chain amino acids) in blood samples have been associated with a twofold increased risk of a pancreatic diagnosis.
This indicates that an increase in the breakdown of proteins in the body may be an early indication of pancreatic adenocarcinoma. Increased levels of branched chain amino acids have been previously associated with those who are obese or those who have insulin resistance. Pancreatic cancer has also been linked to changes in metabolism, such as obesity and glucose intolerance.
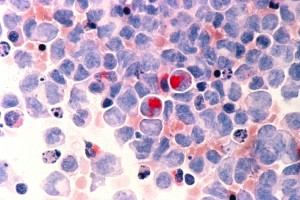
Human cells with acute myelocytic leukemia (AML) in the pericardial fluid, shown with an esterase stain at 400x (Courtesy of the National Cancer Institute)
In addition, advanced pancreatic cancer is strongly linked to cancer cachexia, also referred to as wasting syndrome. Pancreatic tumors have been shown to use amino acids to support their growth, but whether the same is true of branched chain amino acids is not yet clear. The DF/BWCC research team will next investigate whether breakdown of muscle provides a source of branch chain or other amino acids for pancreatic tumors, as well as the timing of this process during pancreatic cancer development.
New Genotyping Technologies
While a tumor biopsy is often the best method of evaluating genomic changes in a tumor, surgical biopsies are not always available. Researchers at the DF/BWCC Lowe Center for Thoracic Oncology are developing a simple, non-invasive blood test to read the genetic abnormalities of a tumor.
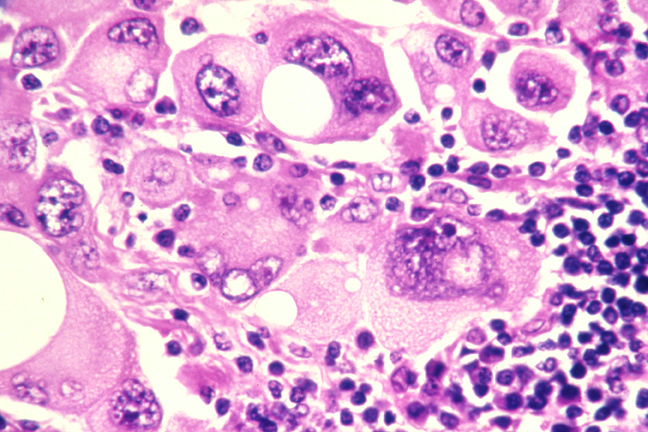
Human metastatic melanoma cells stained with an H & E stain and magnified to 320x (Courtesy of the National Cancer Institute)
Known as plasma genotyping, this technique utilizes free-floating tumor DNA in a patient’s bloodstream to analyze the genetic composition of a tumor. Because it can be performed quickly, plasma genotyping may enable physicians to track the emergence of new gene mutations and promptly prescribe the appropriate targeted therapies. The quantitative nature of the technique may also allow for better monitoring of responses to treatment.
In a recent study, researchers tested the technique in 45 patients with advanced non-small cell lung cancer (NSCLC) whose tumors had become resistant to the drug erlotinib. They found that the plasma genotyping assay was able to detect the relevant mutation 95 percent of the time. Data suggests that this assay is capable of initially providing clinically useful results, while also providing insight into whether a treatment is working.



